Some of the biggest benefits of technology have come in the areas of precision surgery and e-Health provisioning
Technology has opened up new frontiers in the field of medicine and has brought about a rapid change in the areas of diagnostic imaging, minimally invasive surgical techniques, reconstruction and regeneration. This has ushered in a new era of personalised medicines, attaining the digital frontier of e-Health and research.
Diagnostic imaging, with advancement of technology, has shifted from showing anatomical images to functional assessment in situ. For example, fusion of CT MRI images with ultrasound images helps in better characterisation of tumours. The fusion of images makes it possible for much more accurate needle guidance for studying a biopsy specimen.

Minimally invasive surgical techniques are of various flavours. These are endo, robotic, hybrid and stereotactic radiosurgery.
With endo surgical techniques, surgery has ‘taken the fingers of a surgeon outside the body’ through a one-centimeter keyhole incision, which reduces hospital stay and hospital cost. Benefits to the patients include quicker recovery and lesser pain.

Robotics assisted surgery is reliable and has great opportunity in prostrate, obstetric and gynecological surgeries.
Hybrid surgical techniques combine the best options of intervention techniques and surgery for optimising outcomes. Hybrid Cath Labs and OTs help in the delivery of this fusion.
In stereotactic radio surgery, precisely focused radiation is used for treatment without any incision or general anaesthesia for adults. In effect, it is a surgery without a scalpel and hence the name radio surgery. It can be used for treating both malignant and benign tumours.
Reconstruction and regeneration
Reconstruction surgery attempts to restore the anatomy or the function of the body part to normal. This ranges from very simple techniques such as primary closure and dressings to more complex skin grafts, tissue expansion and free flaps. Reconstructive surgery, even when elected for aesthetic reasons, is usually done to correct an abnormality. With advanced technology support like 3D reconstruction and virtual environment technologies and extensive usage of software integrating laser images with computer tomography scan has brought in an edge to reconstructive surgeries. One of the most pervasive uses of reconstructive surgery is in professional sports in addition to cosmetic surgeries and reconstructive surgeries for oncology patients. Many of these procedures are constantly being improved.
Regeneration is a process of creating living, functional tissues to repair or replace tissue or organ function lost due to damage, or congenital defects. This field holds the promise of regenerating damaged tissues and organs in the body by stimulating previously irreparable organs to heal themselves. Regenerative medicine also empowers scientists to grow tissues and organs in the laboratory and safely implant them when the body cannot heal itself. Importantly, regenerative medicine has the potential to solve the problem of the shortage of organs available for donation compared to the number of patients that require life-saving organ transplantation, as well as solve the problem of organ transplant rejection, since the organ’s cells will match that of the patient. For example, this technology is used for growing bone tissues with its own blood supply or in amniotic fluid stem cell for tissue regeneration for treatment of diabetes, cardiovascular repair and repair of central nervous system.
New era of personalised medicines
This is the area of products and services that leverage the science of genomics and proteomics (directly or indirectly) and capitalise on the trends toward wellness and consumerism to enable tailored approaches to prevention and care. Advances in a number of molecular profiling technologies like proteomic profiling, metabolomic analysis and genetic testing allow for a greater degree of personalised medicine. Information about a patient’s proteinaceous, genetic and metabolic profile could be used to tailor medical care to that individual’s needs. A key attribute of this medical model is the development of companion diagnostics, whereby molecular assays that measure levels of proteins, genes or specific mutations are used to provide a specific therapy for an individual’s condition by stratifying disease status, and by selecting the proper medication and tailoring dosages to that patient’s specific needs. Additionally, such methods can be used to assess a patient’s risk factor for a number of conditions and to tailor individual preventative treatments.
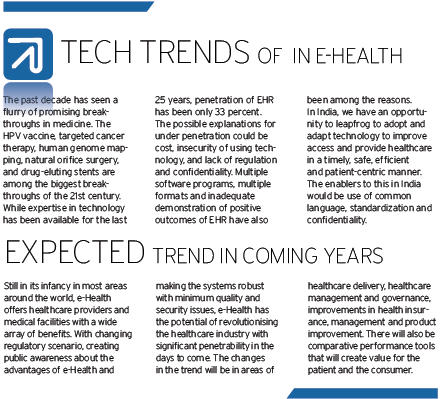
Digital frontier of e-Health
Telemedicine, with the support of IP telephony, has made healthcare accessible to the rural population in the remote corners of the country. Through telemedicine, doctors in the cities can provide consultation to people in the remote villages and can even interpret the ECG and other diagnostic reports. With the new technologies enabling faster transmission of information and images, storage of huge amount of data to be retrieved as needed and lowering the cost, telemedicine is gaining popularity and becoming affordable.
Globalisation of image interpretation is also an area of e-Health. Healthcare providers are under pressure to handle increasing demand for interpretation of medical images. In the face of unequal distribution of expertise across the globe, the need to have technologies to support image transmission to remote locations became pressing.
The demanding consumer put additional pressure for quick turnaround of image interpretation and other diagnostic tests. To overcome this problem, the job of radiology and pathology image interpretation has been globalised with the help of technology. With the new technologies such as cloud, 3G, lower transmission and storage costs, coupled with the new generation Electronic Health Records (EHR) systems, globalisation of image interpretation is fast becoming the practice across the globe.
In our hospitals today, we are already equipped to support remote second opinion from a specialist, with the help of technology. This, along with high-speed network, enables us to effectively use domain specialist clinicians across for collaboration and second opinion on patients, especially for telepathology in the fields of histopathology, oncopathology, bone marrow smears and FNAC studies. For example, motorised microscopes can be used in real time and manoeuvred from remote location by users to see content of a field.
Technology also improves efficiency by providing clinicians with information about their patients at the point of care. Healthcare providers and facilities can deliver better quality of care and a more satisfying patient experience.
e-Health offers a mechanism that eliminates duplication of efforts and provides operational and administrative efficiencies, reducing costs.
The area of research
The increased longevity of humans over the past century can be significantly attributed to advances resulting from medical research. Among the major benefits have been vaccines for measles and polio, insulin treatment for diabetes, classes of antibiotics for treating a host of maladies, medication for high blood pressure, improved treatments for AIDS, statins and other treatments for atherosclerosis, new surgical techniques such as microsurgery, and increasingly successful treatments for cancer. New, beneficial tests and treatments are expected as a result of the human genome project.
Many challenges remain, however, including the appearance of antibiotic resistance and the obesity epidemic.
Be a part of Elets Collaborative Initiatives. Join Us for Upcoming Events and explore business opportunities. Like us on Facebook , connect with us on LinkedIn and follow us on Twitter, Instagram.











